The role of prolactin in the female body
Under the influence of prolactin in women, colostrum matures, which turns into mature milk.
Effects of mammotropin:
- enhances colostrum production;
- participates in the growth and development of the mammary glands;
- helps to increase the number of lobules in the chest and ducts;
- ensures that the glands are filled with milk until subsequent feedings;
- in pregnant women, regulates the amount and composition of amniotic fluid;
- affects the synthesis of progesterone by the corpus luteum during pregnancy;
- responsible for slowing down ovulation and new conception;
- prevents pregnancy and the onset of menstruation during lactation;
- ensures immunological tolerance of the embryo during pregnancy;
- when prolactin levels increase, an analgesic effect is observed; when it decreases, sensitivity to pain increases;
- participates in the formation of the internal lining of the pulmonary alveoli;
- slows down the secretion of gonadotropin-releasing factor and folliculotropin;
- reduces estrogen production;
- helps prolong the luteal phase of the cycle;
- participates in ensuring sexual satisfaction; hormone levels may be an indicator of orgasm;
- affects lipid metabolism, kidney function, and immunity;
- participates in immune reactions, has an immunostimulating effect in immune processes;
- stimulates the growth of new blood vessels.
Hormone receptors are present in almost all organs, but their effect on tissue is unknown. Increased synthesis of estrogen during pregnancy and milk production by the mammary glands is possible only with increased prolactin. After childbirth, its level decreases sharply, but its support is provided by nipple receptors.
Why is prolactin elevated?
Among the most common causes of hyperprolactinemia are:
However, finding out the causes of hyperprolactinemia is not so easy: every third case cannot be explained. In such a situation, even if all provoking factors are eliminated, the prolactin level does not disappear. In this case, experts recommend nutritional adjustments and non-hormonal therapy. For example, some substances contained in chasteberry have a gentle effect on the pituitary gland, increasing the level of progesterone, which suppresses the synthesis of prolactin. As a result, the hormonal balance is normalized gently and naturally. Hormonal therapy is resorted to only in cases of severe hyperprolactinemia.
High level reasons
Hyperprolactinemia is of two types: physiological (normal) and pathological. Signs of physiologically increased prolactin are observed in women during intimacy, pregnancy, breastfeeding, nipple stimulation, physical overload, stress, during deep sleep, and during meals. The maximum physiological level of prolactin is achieved during REM sleep or in the early morning hours. Pathological hyperprolactinemia is associated with disease.
High prolactin values can be criteria for the following diseases or conditions in a woman:
- amenorrhea;
- galactorrhea (including in men);
- ovarian dysfunction, Stein-Leventhal syndrome;
- pathologies of the uterus (endometriosis, fibroids);
- frequent surgical curettage of the endometrium;
- dysfunction of the hypothalamic-pituitary complex;
- Pituitary tumors are benign or malignant. With adenomas, several hormones can be produced simultaneously;
- cirrhosis;
- renal failure;
- hypothyroidism;
- autoimmune disorders (diffuse goiter, rheumatoid arthritis, systemic lupus);
- vitamin B6 deficiency;
- stressful situations;
- insomnia;
- overwork;
- excessive loads;
- tuberculosis;
- activation of immunity during inflammatory processes;
- trauma or surgery on the chest or mammary glands.
The cause of high prolactin may be taking certain groups of medications:
- antihistamines;
- neuroleptics;
- estrogen-containing drugs;
- antiemetics;
- painkillers;
- hypotensive;
- antidepressants;
- oral contraceptives.
There is also a third form of hyperprolactinemia (idiopathic), the causes of which are unknown. In this case, the functions of pituitary cells are increased, but their number does not change.
An insignificant reason, for example, fear of medical procedures, can increase the level of the hormone. In this case, the analysis is performed repeatedly.
Causes of hyperprolactinemia
If you have both excess weight and hyperprolactinemia, you should first find out the cause of the latter. Only after its elimination can you begin losing weight, otherwise it will be useless.
Physiological reasons:
- deep dream;
- intense physical activity;
- lactation;
- pregnancy;
- age-related changes in the body after 40 years;
- menopause;
- taking certain medications (hormonal, antipsychotic, antihistamine, antiemetic);
- sexual intercourse
Pathological reasons:
- galactorrhea;
- amenorrhea;
- gynecological pathologies;
- dysfunction of parts of the brain;
- hypothyroidism;
- renal failure;
- cirrhosis of the liver;
- autoimmune diseases;
- vitamin B6 deficiency;
- stress;
- mammary gland injuries;
- frequent abortions, intrauterine device.
Elevated prolactin levels due to physiology are temporary. In this case, there is no need to sound the alarm and immediately stop breastfeeding or deny your partner sex just to get rid of excess weight. You need to wait out these surges and everything will return to normal on its own.
But for pathological reasons, you will have to go to the doctor and get treatment, otherwise no diet, even the most effective one, will help you lose weight.
Did you know that... increased mammotropin carries not only harm, but also benefit? For example, it can cure multiple sclerosis.
Norm prolactin in women
Mammotropin is produced according to the feedback principle. Inhibition of its secretion occurs under the influence of the neurotransmitter dopamine, which is formed in the hypothalamus. When the formation of dopamine ceases, an increase in prolactin is observed under the influence of estrogens in the blood. With an increased concentration of estrogen, increased stimulation of the formation of lactotroph cells occurs. There are different units of measurement for lactotropic hormone. Its level depends on the woman’s age, gestational period, menstrual cycle, whether she is breastfeeding or not, as well as an increase due to illness.
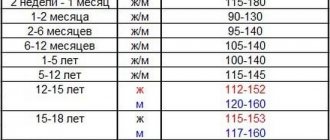
Norms by age category
| Age (years) | Indicator (ng/ml) |
| 16-18 | 2,1-18,4 |
| Over 18 | 6,0-27,0 |
| Menopause | 1,2-18,8 |
According to the menstrual cycle
| Cyclic phase | Normal (ng/ml) |
| Folliculin | 4,5-27 |
| Ovulatory | 6,3-45 |
| Luteal | 4,9-40 |
In pregnant women and during lactation
| Gestation period (in weeks) | Normal (ng/ml) |
| Until 13th | 3,2-43 |
| Until 13th | 3,2-43 |
| 13-24 | 13,0-166 |
| After the 24th | 13,0-318 |
| Breastfeeding up to 6 months | 47,6-57,1 |
| Feeding after 6 months | Up to 119 |
During pregnancy, prolactin in women increases 10-20 times. Its high levels should be maintained throughout the entire lactation period.
The importance of prolactin in the regulation of the female reproductive system
Among the variety of causes leading to disruption of the full function of the ovaries and, as a result, endocrine infertility due to the lack of ovulation, the phenomenon of hyperprolactinemia occupies a special place.
Hyperprolactinemia is an increased level of prolactin (one of the most important hormones of the pituitary gland) in the blood serum.
Prolactin is a unique hormone that has more than three hundred different biological effects. The main site of prolactin synthesis is the adenohypophysis, one of the most important organs regulating the function of the endocrine glands, located in the brain. It is interesting to note that in addition to the pituitary gland, prolactin can be synthesized in other organs: in the mammary and lacrimal glands, myometrium (uterine muscles), spleen, skin, lymph nodes and bone marrow. Receptors that perceive its signal are scattered throughout almost the entire body, including the organs of the immune system. The spectrum of action of prolactin is wider than the total of all other pituitary hormones.
The influence of prolactin on the organs of the reproductive system is manifested at almost all levels of regulation. Thus, even during puberty, prolactin ensures the processes of growth and structural development of the mammary gland. In the ovaries, thanks to prolactin, the processes of follicle maturation and ovulation are synchronized. In the uterus, prolactin increases the number of receptors for progesterone and estrogen, and has a beneficial effect on the process of embryo implantation. Thus, it is impossible to underestimate the importance of prolactin in the regulation of the reproductive system. However, the main role of this unique hormone is the stimulation of milk synthesis by the glandular tissue of the mammary glands, which manifests itself after childbirth, when there is a physiological increase in the level of prolactin in the blood.
Thus, if for a number of reasons (injuries and neoplasms in the brain, taking certain medications, breastfeeding, stress, etc.) the level of prolactin in the blood serum exceeds physiological values, then this has an extremely negative effect on reproductive function. This phenomenon has been known since the time of Hippocrates. In his famous treatises, he Fr.
It should be noted that decreased function of the thyroid gland (hypothyroidism) can also be accompanied by an increase in the level of prolactin (thyroid hormone-releasing hormone in increased quantities stimulates the synthesis of thyroid-stimulating hormone and prolactin due to the cross-effect), therefore it is extremely important, for various disorders of the menstrual cycle, along with prolactin, to determine and serum thyroid-stimulating hormone (TSH) level.
An increase in prolactin levels may be primary when the cause is the increased function of lactotrophs (cells in the pituitary gland that produce prolactin) or an increase in their number, which occurs with pituitary tumors (prolactinoma). There are also secondary forms of hyperprolactinemia associated with various diseases and neoplasms in the brain, taking medications that indirectly stimulate the formation of prolactin (oral contraceptives, cerucal, methyldopa, halaperidol, etc.).
When should you think about possible disorders of prolactin synthesis?
First of all, with an irregular menstrual cycle. Most often, an increase in the level of prolactin in the blood provokes delays, and in more severe cases, a complete cessation of menstruation. In addition, if a woman experiences discharge from the mammary glands in the form of colostrum, which increases with pressure, or lactorrhea (spontaneous milk release), she should immediately consult a specialist. The minimum list of examinations should include: determining the content of prolactin and TSH in the blood, conducting an ultrasound (in women under 35 years old) or x-ray examination of the mammary glands.
It should be noted that even if a woman maintains the rhythm of menstruation, and pregnancy does not occur, it is necessary, first of all, to determine the content of prolactin in the blood serum.
Depending on the level of prolactin, the doctor decides on the advisability of performing MRI of the brain in order to exclude a hormonally active tumor of the pituitary gland - prolactinoma. As a rule, micro (up to 1 cm) and macroprolactinomas (more than 1 cm) are accompanied by a significant increase in prolactin content in the blood (over 1500-2000 mIU/l). Less significant increases may indicate functional hyperprolactinemia.
In this regard, it is very important to conduct at least three hormone studies with an interval of several days and preferably at the same time.
If the diagnosis of hyperprolactinemia is confirmed, then before planning a pregnancy it is necessary to undergo a course of drug therapy aimed at normalizing prolactin levels. The duration of the therapeutic effect is always individual, but, as a rule, 3-6 months of stable compensation is sufficient. If the increase in prolactin is caused by a pituitary adenoma, then the need for specific therapy remains throughout both the period of preparation for pregnancy and the entire period of gestation and lactation.
Finally, it should be noted that the phenomenon of “Macroprolactinemia”
. This is an exclusively laboratory phenomenon, due to the fact that elevated titers of prolactin are determined in the patient’s blood, and any clinical symptoms are completely absent. This phenomenon may be caused by the fact that the increase in hormone levels is caused by biologically low active “big” and “big-big” prolactin with a high molecular weight. In this case, no medications need to be taken.
Prolactin has a fairly pronounced circadian rhythm with the maximum release of the hormone during night sleep. Therefore, blood is taken for analysis in the morning, no earlier than 3 hours after waking up. Standard values of prolactin in blood serum in women range from 67 to 726 mIU/l;
Before conducting the study, it is necessary to: exclude sexual contact and heat exposure (sauna) 1 day before, and smoking 1 hour before. Because Stressful situations have a great influence on prolactin levels; it is advisable to exclude factors that influence the research results: physical stress (running, climbing stairs), emotional arousal, sleepless night, etc.
Author of the article
: gynecologist-reproductologist, Ph.D. Belokon Irina Petrovna
Symptoms
Women make the most complaints about hyperprolactinemia during the active reproductive period of life (25-35 years). This is mainly due to the fact that with increased prolactin, menstrual function suffers more. One of the characteristic symptoms is galactorrhea, when milk is secreted outside the lactation phase. The symptom is typical for 40% of women with elevated prolactin.
Galactorrhea is classified into three degrees of severity:
- The first is that with slight compression of the chest, a few drops appear.
- The second is that upon palpation, milk flows in thin streams.
- The third is spontaneous leakage of milk without pressure on the mammary glands.
Don't self-medicate
Contact our specialists who will correctly diagnose and prescribe treatment.
Other signs:
- scanty periods up to amenorrhea;
- metrorrhagia;
- irregular menstruation, frequent delays;
- bleeding outside the cycle;
- masculinization (a woman develops secondary male sexual characteristics). Against the background of masculinization, there may be an increase in sexual desire;
- Excessive greasiness of the skin on the face and hair. The appearance of acne, deterioration of the elasticity of the skin;
- weight gain for no apparent reason;
- blood pressure surges;
- dizziness, headaches;
- fatigue, persistent insomnia, depression, psycho-emotional instability. Too high prolactin levels can cause mental illness;
- dryness of the vaginal mucosa;
- prolongation of menopause by several months or years;
- thyroid dysfunction occurs due to hormonal imbalance;
- insulin tolerance and increase in its concentration in the blood;
- breast tenderness, breast enlargement up to macromastia. With highly elevated prolactin, cysts form in the glands, which subsequently leads to mastopathy and cancer;
- decreased libido up to frigidity;
- anorgasmia;
- the formation of prolactinoma (benign cancer), leading to blindness due to compression of the optic nerves;
- memory impairment.
With prolonged elevated prolactin, calcium metabolism is disrupted, which is washed out of bone tissue. Due to a lack of calcium and estrogen, bone density decreases, which leads to osteoporosis (brittle bones).
Prolactin in men
Normally, this hormone should be slightly lower compared to the female body. Prolactin is necessary for the production of another hormone - testosterone (only with normal levels of this hormone do sperm develop correctly and perform their function).
In addition, prolactin supports a man’s immunity, is responsible for his body weight, and also takes part in the formation of secondary sexual characteristics.
REFERENCE!
High levels of the hormone lead to the appearance of female secondary sexual characteristics in a man, including female-type breast growth.
Diagnosis of hyperprolactinemia
Hyperprolactinemia can be suspected if there is a combination of pathologies: uterine fibroids, galactorrhea, mastopathy. This triad is typical when prolactin levels increase. But often a woman’s only complaint may be a lack of regulation or another pronounced cycle disorder. Amenorrhea is the leading sign in identifying hyperprolactinemia. The doctor interviews the woman, collects anamnesis, identifies other symptoms, and conducts an examination.
A blood test is prescribed to determine hormone levels for the following indications:
- cycle disorder;
- delayed sexual development;
- secretion of colostrum or milk in non-lactating women;
- unable to get pregnant;
- lack of postpartum lactation;
- blurred vision;
- history of pituitary tumors;
- after operations in the hypothalamic-pituitary system.
For analysis, venous blood is taken in the morning on an empty stomach, no earlier than an hour and a half after sleep. You should not smoke before donating blood. 1-2 days before the procedure, you should not overexert yourself physically, touch or put pressure on your breasts, avoid sexual contact, and do not take a hot bath. You need to maintain emotional balance.
The optimal timing is 5-7 days of the cycle. The analysis is done 3 times on different days, which are prescribed by the doctor, in the same laboratory.
To establish the level of prolactin and determine the reasons for its increase, the following diagnostics are performed:
- thyroid hormones;
- blood for glucose;
- cholesterol analysis in obese patients;
- X-ray of the skull to study the sella turcica;
- CT or MRI if cancer of the hypothalamus or pituitary gland is suspected;
- transvaginal ultrasonography (abdominal in pregnant women) to assess the condition of the woman’s pelvic organs;
- An ophthalmologist is consulted to determine the visual fields and identify changes in the fundus.
Which hormone is to blame for obesity? The role of prolactin in excess weight gain.
Recently, doctors are increasingly talking about the relationship between obesity and increased levels of prolactin, a hormone produced by the cells of the anterior pituitary gland. We already know that all troubles come from the head. But how exactly do the features of the brain affect the increase in body size? Is it possible to somehow control these processes from the outside? With this and other questions, the magazine “Pro Health” turned to Irina KUZNETSOVA, Doctor of Medical Sciences, gynecologist-endocrinologist, professor of the Department of Obstetrics and Gynecology of the Russian Medical Academy of Postgraduate Education . – What is this mysterious prolactin and what is its role in the body?
– Oh, this is a completely mysterious hormone. He is the only one who intervenes in all processes, but his role for our health, meanwhile, is not fully understood. Its absolute importance for the formation of lactation is known; without prolactin, a woman cannot produce milk. But what he does while participating in other “scenarios” of our lives is not yet clear to scientists. We know that prolactin can affect the reproductive system, the bone system, and metabolism; it is also one of the adaptogens - it is released into the blood in response to stress and helps the body withstand excess physical or mental stress. But what metabolic processes does it trigger? For now, we can only state that prolactin increases for some reasons known only to it. Although the regulators of prolactin levels in the brain are well known. This is dopamine, which controls (reduces) prolactin production. The second regulator is thyrotropin-releasing hormone, a hormone that increases the production of thyroid-stimulating hormone (TSH) and, for company, prolactin. That is why, with hypofunction of the thyroid gland, prolactin can increase simultaneously with TSH. Prolactin levels also increase during sex, which is why doctors always warn patients not to have sexual intercourse before taking tests. But what role does he play in this? No one has explored it yet...
– Perhaps it, as an adaptogen, prevents us from dying of love...
– Or helps to enjoy it... Everything is possible, but not proven. This is a hormone that, on the one hand, helps everyone everywhere and, on the other hand, is always on its own. Much more is known about other hormones. For example, adrenocorticotropic hormone (ACTH), like prolactin, is a hormone of the anterior pituitary gland. It stimulates the function of the adrenal cortex. Thyroid-stimulating hormone increases the function of the thyroid gland, follicle-stimulating hormone regulates the activity of the gonads, forms the function of the ovaries, etc. And only prolactin does not initiate or stimulate anything. He is probably the only one that acts on his own, and not through some “intermediaries.” And at the same time directly - on tissues, adrenal glands, ovaries, peripheral endocrine glands. Perhaps this is a wise quirk of nature. And she very wisely insured us for various occasions. If some hormone doesn’t cope, here’s prolactin to help you. He can work “on all fronts” and with very multidirectional effects. But at the same time unpredictable. It is never known, for example, if prolactin is high, there will be some kind of menstrual irregularity or not. With the same excess weight. Against this background, someone will gain weight, and someone will lose weight. The body's reaction to prolactin is very individual and depends on the characteristics of the hormonal background. Today, only one thing can be said with certainty: when it comes to prolactin, there is always an ellipsis.
– If everything is so vague, why then are we women, as soon as the doctor notices some problems in the reproductive system, immediately forced to take tests for prolactin?
– Although the mechanisms of action of many processes are still completely unknown, doctors know that hyperprolactinemia (a persistent increase in prolactin levels) is a signal of disorders, sometimes very serious, especially in a woman’s body. And the first target of a pathological increase in prolactin levels is precisely the reproductive system. First of all, this is infertility, amenorrhea (lack of menstruation). If a non-pregnant woman of fertile age does not have or has stopped menstruating, in 70% of cases we find elevated prolactin levels. Also, women and girls experience insufficiency of phase II of the menstrual cycle, delayed menstruation, ovulation disorders, and the release of colostrum or milk from the mammary glands in the absence of pregnancy and childbirth. With hypothyroidism and increased prolactin in girls, the mammary glands begin to develop prematurely. Fibrocystic mastopathy also often occurs against the background of an increase in the amount of this hormone. Another danger that high prolactin may signal is a disruption of the endocrine balance with the formation of hyperandrogenism (increased production of male sex hormones or increased sensitivity of tissues to them). For women, this is a visceral increase in fat and increased hair growth. But not only. These are also risks from the heart, blood vessels, and metabolic syndrome. The autonomic nervous system will also suffer, since prolactin is an adaptogen. Patients may feel hot flashes, palpitations, trembling hands, sweating, and dry skin. In the end, the process becomes somatized and results in a disease, sometimes cancer with the growth of tumors, and mental abnormalities may also appear.
– Can a hormone cause cancer?
– Let's try to explain everything from the point of view of physiology and pathophysiology. Stress is not just something we worry about. This is a whole chain of processes in the body. As we remember, the notorious adaptogen prolactin is released in response to stress. The more we experience, the higher its level. This is how the body reacts, mobilizing all its defenses. If stress is chronic, the body's reserves will gradually be depleted. The cell will suffer and will not have time to control what is happening in it. This would upset the balance of life and death in her life cycle. She will survive against all odds, but will start a pathological process. This is how cancer usually develops.
- Let's go back to obesity. Why does modern medicine associate the appearance of excess weight with prolactin? And why do experts convince us that if you are overweight, you must lower your hormone levels and take hormonal medications?
– Everything here is both complicated and simple. The fact is that with obesity it is never completely clear: excess weight forms hyperprolactenemia, or an increase in prolactin is formed as a result of dysfunction of the hypothalamic-pituitary system in response to increased weight. But, be that as it may, we cannot equate obesity and prolactin. 95% of obesity is still overeating, 5% is due to hormonal reasons. Among these 5% there is not only hyperprolactinemia. Obesity must be treated, first of all, with diet and lifestyle correction. Hormonal drugs in this case are in last place. But if during obesity we observe a persistent increase in prolactin levels, it needs to be reduced in any case, because we know how much trouble can happen if it goes off scale. This is where special medications are required. By the way, high levels of prolactin also interfere with the process of weight loss. Diet and exercise simply won't work and help you lose weight.
– For what symptoms should you go and get tested for prolactin?
– If your body mass index is 30 or more. For any menstrual irregularities. In the event that autonomic dysfunction syndrome reminds you of itself (we talked about the manifestations above). An analysis for prolactin is also necessary for osteoporosis if it is detected in a young woman. The reason to visit the laboratory should be any pathology of the mammary glands, infertility, increased hair growth, impaired visual fields and other neurological symptoms, psycho-emotional disorders, including premenstrual syndrome in women. In men, elevated prolactin levels often accompany infertility and decreased libido. In children and adolescents – delayed sexual development. And based on the test results, your endocrinologist will prescribe which medications to take and in what quantity.
PsyAndNeuro.ru
Prolactin (PRL) is a single-chain polypeptide hormone. It is synthesized in the adenohypophysis, endometrium, decidua, lymphocytes, mammary gland and prostate. Produced outside the central nervous system, PRL acts as a cytokine. The release of PRL is cyclical and occurs with a frequency of once every 95 minutes, with the largest amount observed during sleep and the smallest during the daytime.
The synthesis of prolactin is stimulated by liberins, these include vasoactive small intestinal peptide, thyroliberin, prolactoliberin. In addition, the formation of prolactin is stimulated by estrogens and other sex hormones, produced in large quantities during pregnancy, the postpartum period and lactation. Serotonin and melatonin stimulate the production of PRL by the pituitary gland, which has been proven when they are injected into the third ventricle of the brain.
Regulation of production is carried out from the arcuate nucleus of the hypothalamus along the tuberoinfundibular pathway. Dopaminergic neurons have an inhibitory effect on prolactotrophs, thereby reducing the amount of prolactin. Dopamine is able not only to reduce release, but also synthesis, which leads to the disappearance of secretory granules and, therefore, for some time reduces the release of the hormone even when exposed to a stimulating signal. In addition to dopamine, GABA and somatostatin have an inhibitory effect.
Due to its structure, PRL is not able to freely penetrate into the cell, so its receptors are located on the surface of the membrane. When interacting with them, a cascade of reactions is triggered, leading to the activation of cAMP. The main target for PRL is the mammary gland. Under the influence of the hormone, its cells divide more actively, increase in size, galactogenesis is stimulated in them and, as a result, galactorrhea. In the ovaries, PRL inhibits ovulation, prolongs the life of the corpus luteum, and determines the balance of ovarian estrogens, which contribute to the maintenance of pregnancy. Receptors are also located on the cells of the heart, lungs, thymus, liver, spleen, pancreas, kidneys, adrenal glands, uterus, muscles, skin and central nervous system.
PRL regulates the reproductive and immune systems, angiogenesis, energy metabolism, osmotic balance and more. In the central nervous system it has an anxiolytic effect, inhibits the HPA axis and the neuropituitary oxytocin system. May counteract glucocorticoid effects during stress.
The concentration of PRL in the blood can change either in the direction of its increase or decrease, and accordingly such pathological conditions as hyperprolactinemia and hypoprolactinemia arise.
Hypoprolactinemia occurs with Sheehan syndrome, post-term pregnancy, and taking medications, for example, dopamine agonists. It is relatively rare in psychiatric practice.
Hyperprolactinemia is of great importance, as it is a common side effect when taking antipsychotic drugs. In clinical practice, it can develop with hormonally active pituitary tumors, infections, and infiltrative processes of the gland. In addition, secondary hypothyroidism, ectopic secretion of hormones, polycystic ovary syndrome, severe somatic conditions can also lead to a persistent or transient increase in PRL in the blood.
Hyperprolactinemia is manifested by menstrual irregularities, including amenorrhea, infertility, psycho-emotional disorders (often in the form of depressive symptoms), obesity, excess hair growth in women, impotence and erectile dysfunction in men.
Drugs that primarily affect the dopaminergic system of the brain can alter prolactin metabolism. Antagonists of dopamine and serotonin receptors, which primarily include antipsychotics, inhibit the release of dopamine and reduce its concentration in the synaptic cleft, thus weakening the inhibitory effect of the neurotransmitter on the synthesis and release of PRL, which leads to hyperprolactinemia.
Correction of hyperprolactinemia when taking antipsychotics can be carried out in several ways - by selecting the minimum effective dosage of an antipsychotic, switching to a drug with a lower risk of developing this pathology, or prescribing a corrector from the group of dopamine receptor agonists.
Also extremely interesting is the role of PRL as a stress-adaptive hormone that regulates many emotional and neuroendocrine stress responses in the brain. In the central nervous system, PRL has an anxiolytic effect, as well as an inhibitory effect on the HPA axis and the neuropituitary oxytocin system.
PRL is released from the pituitary gland in response to a number of stressors. Early research suggests that PRL may counteract the glucocorticoid effects on the immune system during stress. Later work found that reducing PRL receptor expression in the brain of virgin and lactating rats significantly increased stress-induced ACTH secretion, indicating for the first time that PRL has an inhibitory effect on the HPA axis. Moreover, intracerebroventricular administration of PRL to virgin female rats reduces amygdala neuronal activation and CRH expression in response to stress.
Induced hyperprolactinemia in adult male rats has an antidepressant effect in the forced swim test. However, there are some differences between people: some patients with hyperprolactinemia exhibit depressive symptoms. However, there was no difference in the prevalence of depression in patients with hyperprolactinemia compared with controls.
Prepared by: Zhukova S.O., Kasyanov E.D.
Sources:
1. Luz Torner. Actions of Prolactin in the Brain: From Physiological Adaptations to Stress and Neurogenesis to Psychopathology. FrontEndocrinol (Lausanne). 2016; 7: 25.2. 2.
2. Torner L, Neumann ID. The brain prolactin system: involvement in stress response adaptations in lactation. Stress. 2002 Dec;5(4):249-57.3.
3. Gala RR. The physiology and mechanisms of the stress-induced changes in prolactin secretion in the rat. LifeSci. 1990; 46(20):1407-20.4.
4. Barishpolets V.V., Fedotova Yu.O., Sapronov N.S. Structural and functional organization of the dopaminergic system of the brain. G. Experimental and clinical pharmacology. T.72. No. 3. Pages 44-49. 20095.
5. Gorobets L.N. Neuroendocrine dysfunctions in patients with schizophrenia. / J. Social and clinical psychiatry. T.15. No. 1. Pages 89-99. 20056.
6. Gorobets L.N., Mazo G.E. Drug correction of neuroleptic hyperprolactinemia. Review of psychiatry and medical psychology named after V.M. Bekhterev | No. 2, 20177.
7. Dedov I.I., Melnichenko G.A., Lipatenkova A.K. Modern neuroendocrinology.
8. Lychkova A.E., Puzikov A.M. Prolactin and serotonin / J. Bulletin of the Russian Academy of Medical Sciences. T.69. No. 1-2, pp. 38-45. 2014