Arthrosis is a chronic disease in which progressive degenerative changes occur in the cartilage tissue of the joints. Along with drug therapy and physiotherapy, a complete, balanced diet is important, aimed at providing the body with the necessary nutrients, improving metabolism and slowing down the process of deformation of the joint structure.
If you have
arthrosis of the joints
, then you should regularly
carry out preventive treatment
.
General rules. Duration of the diet.
Nutritional correction for arthrosis has a positive effect on treatment results and improves the patient’s quality of life.
The therapeutic diet for arthrosis imposes certain rules:
- A varied diet. Nutrition should be complete and balanced.
- Limit salt intake to 5-8 grams per day. Smoked meats, canned food and other salty foods are removed from the diet)
- Drinking regime. It is recommended to increase the consumption of non-carbonated mineral water to 2-2.5 liters per day.
- Introduction to the menu of foods rich in vegetable oils, especially unsaturated fatty acids omega-3 and omega-6.
- It is useful to prepare jellies, jellied fish, fruit jellies and jelly. The mucopolysaccharides they contain help normalize the structure of cartilage tissue and stimulate its synthesis.
Arthrosis in athletes
The disease also develops in athletes. The reason for this is the heavy load on the joints during long and grueling workouts .
Most often, arthrosis occurs in people who engage in sports at a professional level: bodybuilding, weightlifting, powerlifting , arm wrestling, but it can also occur in other people of a completely different nature, for example, ballerinas develop arthrosis of the toes over time.
Arthrosis in athletes
The diet for arthrosis in athletes should include:
- Collagen fibers of plant origin
- Vitamins and microelements
- High protein content
- Chondroitin and glucosamine (as a dietary supplement)
What can you do for arthrosis of the joints? List of permitted products.
SOUPS:
Soups made from weak meat and fish broths with the addition of cereals and vegetables.
MEAT:
Low-fat meats Idea, chicken, veal, rabbit.
Jellies and meat aspic. FISH:
River and sea.
Red varieties are preferred. Jellies and fish aspic. DAIRY PRODUCTS:
Low-fat fermented milk and fermented milk products - kefir, fermented baked milk, yogurt, as well as lean cheese, dietary cottage cheese and yogurt.
BREAD:
Wholemeal and wholemeal breads.
VEGETABLES:
Almost any vegetables are allowed, both raw and thermally processed.
It is necessary to minimize the consumption of tomatoes. It is recommended to add flax and sesame seeds to salads. FRUIT:
Almost all types of fruit are allowed, but in small quantities.
Jelly made from natural fruits and berries is recommended. DRINKS:
Compotes, decoctions, green tea with lemon, fruit juice, alkaline mineral water.
Diet for arthrosis - what doctors recommend
It is believed that jellied meat or jelly prepared on the basis of bone broth is useful arthrosis This broth contains a large amount of collagen, which is necessary for the construction of cartilage and bone tissue, muscles and ligaments. Edible gelatin is also useful. The substances it contains - chondroprotectors - help restore cartilage tissue. Proteins are used to build new tissues, including the restoration of cartilage tissue covering the articular surfaces of bones. Dairy products are especially useful for restoring joints. Milk protein is easily absorbed by the body; in addition, dairy products (especially cottage cheese and cheeses) contain a lot of calcium, which is necessary to strengthen bone tissue. Animal protein is found in lean meat and fish, vegetable protein is found in buckwheat porridge, beans and lentils. To ensure that proteins are better absorbed, it is preferable to include boiled, stewed or steamed dishes in your diet.
Carbohydrates provide the body with the energy necessary for the smooth functioning of metabolic processes. But carbohydrates are different. Simple sugars (sweet and rich foods) are easily absorbed by the body and provide a quick burst of energy, some of which is stored as fat reserves. Complex carbohydrates (found in vegetables and fruits) are absorbed slowly, so they do not turn into fat. This is very important from the point of view of preventing excess weight.
Fats are also necessary; without them, metabolic processes slow down sharply. But the diet of patients with arthrosis should consist mainly of vegetable fats and butter.
Vitamins and minerals are of great importance for proper metabolism. Vitamins of group B are especially useful. Thus, vitamin B1 is found in peas, baked potatoes, whole grain bread, and beans. Vitamin B2 - in dairy products, bananas, eggs, B6 - in bananas, potatoes, chicken meat, nuts. Folic acid (vitamin B12) - in bananas, lentils, cabbage.
The best way to maintain healthy joints is to eat a diet that is low in carbohydrates, limited in protein and calcium, and rich in fruits and vegetables.
What is not allowed for arthrosis of the joints? List of completely or partially restricted products.
SOUPS:
Soups with concentrated meat and fish broths are prohibited.
MEAT:
Fatty varieties of red meat, semi-finished products, smoked meats, and sausages are undesirable.
It is recommended to minimize the consumption of offal (liver, kidneys, heart). FISH:
River and sea.
Fried, smoked or pickled fish is prohibited. DAIRY PRODUCTS:
Sour cream, cream, full-fat cheese.
BREAD:
Bread, yeast baked goods, and high-calorie cream confectionery products are not allowed.
VEGETABLES:
Canned vegetables should not be consumed.
DRINKS:
Alcohol, strong tea and coffee are prohibited.
SPICES, CONDITIONINGS:
Hot spices and seasonings are not allowed.
Principles of nutrition
A balance of nutrients in the daily menu is the main principle of proper nutrition for arthrosis.
This can also include:
- regularity of intake;
- diversity;
- energy value adequate to consumption;
- easy digestibility and absorption;
- large amounts of fluid consumed;
- freshness of preparation.
The number of receptions should be 4-5 times, at a strictly defined time. Dinner should be taken 3.5 hours before bedtime. A variety of foods should provide the musculoskeletal system with useful substances to the fullest. If you are overweight, you need to fight it, since every extra kilogram is a negative load for sore joints.
To solve this problem, you should replace cottage cheese and medium-fat cheese with low-fat cheese. It is also necessary to reduce the amount of bread consumed. For ease of control, you need to know your body mass index. Weight must be divided by height in meters squared.
Normal body mass index = 20-25. For class I obesity – 25–30, class II – 30–40, class III – more than 40.
Proteins and carbohydrates cannot be combined in one dish. Moreover, you should not eat fruit after meat. The speed of fruit digestion is 15–20 minutes. The digestion speed of animal proteins is about 2 hours. Therefore, digested fruits are not evacuated from the stomach until the meat is digested. As a result, fermentation occurs, which leads to indigestion. It is better to eat fruits 30 minutes before meals. Proteins of animal and plant origin should also not be combined in one dish.
Recipes for dietary dishes for arthrosis
(Diet features for adults/children)
Arthrosis of the joints in children is very rare; the disease is more typical in adults aged forty-five years and older. Treatment must be carried out under the supervision of a doctor. Diet recommendations include providing the child with a complete, balanced diet without reducing its nutritional value. In this case, it is necessary to completely exclude such products as smoked meats, sausages and confectionery products (especially cream-containing ones), chips, sweet carbonated drinks, and too fatty dishes.
Arthrosis
22473 08 June
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Arthrosis: causes, symptoms, diagnosis and treatment methods.
Definition
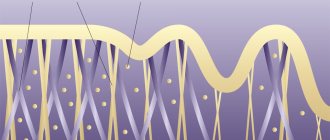
Arthrosis (arthrosis deformans, osteoarthrosis) is a disease of the joints of a degenerative-dystrophic nature with the gradual destruction of cartilage and proliferation of bone tissue. A joint is the articulation of two or more bones. The structural components of the joint include: the articular surfaces, covered with hyaline cartilage, the joint cavity, which contains a small amount of synovial fluid, the joint capsule and the synovial membrane (membrane).
The most common are deforming arthrosis of large joints - arthrosis of the knee joint (gonarthrosis), hip joint (coxarthrosis), and shoulder joint.
Among the small joints, the disease affects the interphalangeal joints of the hands (in people whose work involves performing small, monotonous movements), the metacarpophalangeal joints of the thumbs, and the joints of the spine.
Causes of arthrosis
The development of arthrosis is based on a discrepancy between the mechanical load on the joint and its ability to withstand it. Simply put, with arthrosis, the joints “wear out” under the influence of time, intense loads, and insufficient supply of nutrients. The articular cartilage becomes damaged and becomes thinner, and the affected bones may become slightly misaligned, causing irritation in the joint.
Over time, the cartilage is completely destroyed, the bones begin to rub against each other, and pain occurs.
Arthrosis can be primary, the cause of which is not completely clear, and secondary – arising against the background of various diseases and conditions. Doctors agree that the development of arthrosis occurs as a result of the combined influence of various factors, for example, genetic characteristics, hereditary predisposition, age, excess body weight, sedentary lifestyle, unfavorable working conditions, concomitant diseases, etc. Secondary arthrosis can result from an inflammatory disease joint, dysplasia (congenital underdevelopment of the joint), blood supply disorders. One of the significant factors in the development of secondary osteoarthritis are occupational injuries and microtraumas with ligament rupture and the appearance of joint hypermobility. Knee joints suffer in loaders, wrist joints - in carpenters and mechanics, elbow and shoulder joints - in painters, drivers, miners, arthrosis of small joints of the hands is diagnosed in milkmaids, weavers, ankle joints - in ballerinas.
Classification of the disease
Arthrosis is distinguished depending on which joints are affected (for example, gonarthrosis, coxarthrosis) and the causative factor. Classifications based on the severity of disorders, determined by radiological signs, are widely used.
In the world, the classification according to Kellgren and Lawrence (Kellgren & Lawrence 1957) is most often used, on the basis of which 5 degrees of arthrosis are distinguished:
Grade 0—no signs of arthrosis. Grade 1 - slight narrowing of the joint space. Grade 2 - slight narrowing of the joint space and slight irregularities of the articular surface. Grade 3 - pronounced narrowing of the joint space and significant unevenness of the articular surface. Grade 4 - pronounced narrowing of the joint space and deformation/necrosis of bone tissue in the joint parts.
In Russia, the clinical and radiological classification of N.S. is more popular. Kosinskaya (1961):
Stage I – movements in the joint are slightly limited, slight, indistinct, uneven narrowing of the joint space, initial osteophytes (slight sharpening of the edges of the articular surfaces).
Stage II - limited mobility in the joint, a rough crunching sound when moving, moderate muscle atrophy, a pronounced narrowing of the joint space by 2-3 times compared to the norm, significant osteophytes (pathological growth of bone tissue).
Stage III - deformation of the joint, limitation of its mobility, complete absence of the joint space, deformation and compaction of the articular surfaces of the epiphyses, extensive osteophytes, articular “mice” (fibrous, cartilaginous or osteochondral formations that move freely in the joint cavity), subchondral cysts.
Symptoms of arthrosis
In most cases, arthrosis causes pain and limited movement in the joint. The severity of symptoms depends on the stage of the disease.
At stage I, with arthrosis of the lower extremities, pain occurs during or after walking and goes away with rest. With gonarthrosis, pain appears when going up and down the stairs, and can make itself felt after a long stay on your feet. With arthrosis of the shoulder joint, patients first notice a slight crunch in the joint; pain occurs only when the limb is abducted to its extreme position. Movement in the joint at this stage is usually not limited.
Stage II arthrosis is accompanied by moderate pain, lameness may develop (with arthrosis of the joints of the lower extremities), and muscle wasting. With arthrosis of the shoulder joint, pain occurs when raising the arm above shoulder level; after prolonged physical exertion on the shoulder girdle, pain appears at rest, movements are moderately limited, and muscle wasting develops.
At stage III, the risk of fractures increases significantly as bone tissue loses its properties. The pain is severe and can be constant (even at rest), lameness is present, the joint is unstable, the muscles atrophy, active and passive movements in the joint are significantly limited.
Arthrosis of the spine is accompanied by a feeling of heaviness in the back when performing active activities or staying in a stationary position for a long time. Then there is aching pain, intensifying with movement, crunching, and stiffness of movement.
Diagnosis of arthrosis
To make a diagnosis, the doctor carefully interviews and examines the patient, measures his height and weight. Assess joint function by gait and degree of daily activity (for example, the ability to climb stairs and use public transport, free movement, etc.).
The main method of instrumental diagnostics is radiography of the joint: hip; shoulder/elbow, wrist, knee, ankle; hands; shoulder joint; knee joint, etc.
Nutritionist comments:
Compliance with the doctor’s nutritional instructions leads to a reduction in the load on the limbs and spine, improves the quality of cartilage tissue, and slows down (and even stops) further destruction of the joint.
“The right choice of a sanatorium is a significant step towards maintaining and increasing health. “Gorny” is a resort complex that combines the experience and knowledge of Russian and Soviet balneology. The presence of modern medical equipment and innovative installations, the professionalism of the staff and love for their work will serve as the key to extending longevity,” - head doctor of the sanatorium Alexander Olegovich Karaulov.
Treatment of joint arthrosis
The choice of treatment for joint arthrosis depends on the cause of the disease, its stage and symptoms. In the arsenal of doctors there are:
- medications;
- non-drug treatment;
- surgical techniques.
In addition, the patient is required to strictly follow a diet and adjust their lifestyle to minimize further damage to the joints.
Drug treatment
Prescribing medications for arthrosis has two main goals:
- relieving pain and inflammation;
- restoration of cartilage tissue or, at least, stopping further degeneration.
To alleviate the patient's condition, various types of drugs are used:
- non-steroidal anti-inflammatory drugs: ibuprofen, ketorolac, diclofenac and their analogues in the form of tablets, injections, ointments or suppositories; they relieve pain and inflammation well;
- hormones (corticosteroids): indicated for severe pain and, most often, injected directly into the joint cavity;
- other analgesics, for example, antispasmodic (mydocalm): help reduce pain by relaxing muscles;
It is important to remember: all types of painkillers are used only to alleviate the patient’s condition. They do not affect the condition of cartilage, but when taken for a long time, they accelerate its destruction and cause serious side effects.
The main drugs for joint restoration today are chondroprotectors. They help saturate the cartilage with nutrients, stop degeneration and initiate cell growth processes. The most common remedy in this group is glucosamine and its analogues. They have an effect only at the early and middle stages of the disease and with regular long-term use.
Drugs that improve microcirculation in tissues and antienzyme agents help enhance the effect of chondroprotectors. The former provide a good supply of oxygen and nutrients to the affected area, while the latter slow down the processes of tissue destruction.
The doctor selects specific medications, their dosage and regimen.
Non-drug treatment
Non-drug treatment includes the following methods:
- physiotherapy: shock wave therapy: destroys bone growths and stimulates blood circulation due to ultrasound;
- automated electromyostimulation: exposure to electrical impulses to stimulate muscle contraction;
- ultraphonophoresis: exposure to ultrasound combined with the use of medications;
- ozone therapy: introduction of a special gas mixture into the joint capsule;
Surgery
Most often, the help of a surgeon is required in severe stages of the disease. Depending on the localization of the pathological process and the degree of damage, the following may be prescribed:
- puncture: puncture of the joint with removal of part of the fluid and, according to indications, administration of drugs;
- corrective osteotomy: removal of part of the bone followed by fixation at a different angle to relieve the load on the joint;
- endoprosthetics: replacement of a damaged joint with a prosthesis; used in extremely advanced cases.
Make an appointment
Basic principles of the diet
No special diet has been developed for patients with arthrosis. Overweight patients are recommended to consume about 2000 kilocalories per day. This energy value is achieved by limiting the diet of foods with simple carbohydrates (approximately 250 g) and fats (up to 50 g). You cannot lose weight too quickly, as this is not physiologically justified. Otherwise, body weight will decrease only due to the destruction of muscles and the accelerated excretion of fluid along with vitamins and microelements. In addition, it is not possible to maintain a lower body weight for a long time. What else do nutritionists recommend:
- eat in small portions up to 6 times a day;
- do not eat 3 hours before bedtime to improve and speed up metabolism;
- do not eat monotonously - the body should receive both proteins and fats with carbohydrates;
- Do not add salt to food during cooking, but directly on the table. It is recommended to reduce its consumption to 5 grams per day.
Compliance with the diet must be combined with daily exercise therapy and gymnastics. This will allow you to quickly lose weight, while simultaneously strengthening the muscles and ligamentous-tendon apparatus of the knee.
Stages of the disease
Stage 1 is manifested by “weather aches,” “crunching,” and limited mobility in the joint. Pain may be absent or mild, mainly under the influence of stress.
Stage 2 intensifies the development of symptoms: the joint loses the ability to fully straighten and the elbow freezes in a half-bent position, pain is observed with every movement, swelling and redness may appear with an increase in temperature in the affected area.
Stage 3 of the disease demonstrates arthrosis of the elbow joint in an advanced form. The joint itself can noticeably increase in size due to deformation of internal tissues and the proliferation of osteophytes. Pain is a constant companion of the patient even at rest. The slightest movement of the hand causes a sharp “lumbago”, and as the disease progresses, the elbow may become completely immobilized (ankylosis of the joint).
Important! If the mobility of the joint is limited, no additional effort should be made to bend/straighten it. This practice can lead to complete jamming of the joint and will only worsen the problem.