What is an intragastric balloon?
The balloon is a smooth ball made of high quality silicone rubber. The balloon has a radiopaque valve through which it is filled with water.
BIB balloon in stomach
Bloated
- balloon in the stomach - 1
- Cylinder valve - 2
- Gastric lumen - 3
- Esophagus - 4
- duodenum - 5
The volume of injected liquid is set only once, at the time of installation. You cannot add or remove a little extra liquid. As a rule, the standard volume is administered - 500 ml. This volume is used by most specialists.
Mechanism of action of the cylinder
The presence of a balloon in the stomach leads to the fact that it fills a significant part of its volume. Consequently, the amount of food a person can eat decreases. In addition, an inflated balloon stretches the wall of the stomach, which leads to irritation of satiety receptors. Such irritation leads to an early feeling of satiety.
How long does it take to place the balloon?
The balloon can be placed in the stomach for a maximum of 6 months. After this, it must be removed. This is explained by the fact that the hydrochloric acid present in the gastric juice gradually destroys the balloon, and it wears out. If the patient wants to continue treatment in this way, the old one must be removed and a new balloon placed in its place.
Who can have such a balloon placed in their stomach?
In order to understand who can have a balloon placed in their stomach for weight loss, you need to have an idea of the Body Mass Index.
So, the first group of patients who can have a balloon placed in their stomach are patients with a BMI from 30 to 40. As a rule, these are people who have already tried many times to lose weight in a variety of ways, but could not get sufficient effect. Many of them ask for a surgical operation to put a ring on the stomach, but with such a BMI, it is premature to perform the operation (it should be done when the BMI is 35-40 or higher). It is in such cases, when it is too early to perform the operation, but it is necessary to reduce weight, and the installation of a balloon is used.
Another group of candidates for balloon placement are patients with a BMI of 40 or higher if they are in poor health. Of course, they need to have weight loss surgery, but the risk of surgery is high. Installation of a balloon and weight loss lead to improved health and, accordingly, a reduced risk of surgery. That is, in this case we are talking about preoperative preparation. Sometimes a balloon is placed in obese patients who are undergoing joint surgery (joint replacement for arthrosis), surgery for hernias and other operations. Even a slight weight loss in them leads to a reduction in the risk of any surgery.
Another group of patients are people with a BMI of 40 and above who have extremely severe cardiovascular diseases. Due to severe cardiopulmonary failure, these patients will never undergo surgery.
If they need to achieve rapid and significant weight loss, they can have a balloon placed in their stomach.
Contraindications
Which patients should not have a balloon inserted into their stomach?
- You cannot install a balloon only for cosmetic reasons.
- Balloon installation is contraindicated in patients with a body mass index less than 30 (except in cases where patients have concomitant diseases, the course of which may improve with a decrease in body weight).
- The use of the BIB system is contraindicated in patients who have previously undergone abdominal or gynecological surgery.
- Balloon placement is contraindicated in the presence of inflammatory diseases of the gastrointestinal tract, including esophagitis, gastric and duodenal ulcers, Crohn's disease, and malignant tumors of the stomach.
- Balloon placement is contraindicated in the presence of potential sources of bleeding in the gastrointestinal tract, such as varicose veins of the esophagus and stomach, congenital and acquired telangiectasia, and other congenital anomalies of the gastrointestinal tract, such as atresia and stenosis.
- Balloon placement is contraindicated in the presence of large hiatal hernias.
- Balloon placement is contraindicated in the presence of strictures and diverticula of the pharynx and esophagus.
- Balloon placement is contraindicated if there are other medical problems that may make gastroscopy difficult.
- Also, a contraindication to balloon placement is the presence of mental disorders.
- Balloon placement is contraindicated in the presence of alcoholism and drug addiction.
- Balloon placement is contraindicated for people with low discipline, who cannot follow the prescribed dietary regimen, and cannot come for medical supervision 2 times a month.
- Contraindications include chronic use of aspirin, other anti-inflammatory drugs, steroids, drugs that irritate the stomach, and anticoagulants (medicines that reduce blood clotting).
- A contraindication to balloon placement is pregnancy or breastfeeding.
Installation method
The balloon is installed under gastroscopy control. This is not an operation, but an endoscopic procedure. It is performed under complete anesthesia. The patient may lie on their back or left side, depending on the physician's preference. A special medical dye, methylene blue, is introduced into a container of water intended for inflating the balloon (it is needed for timely recognition of leaks from the balloon). First, a gastroscopy is performed - an examination of the esophagus and stomach for the presence of diseases that may be a contraindication for the installation of a BIB. The balloon is then inserted through the mouth. A syringe is connected to the catheter, and under visual control, the balloon begins to inflate. In this case, the cover in which the cylinder is located is torn, and the cylinder is released. When the balloon is filled to the required volume (500 ml), the catheter is pulled out of the balloon and the valve closes. The balloon becomes a free ball in the lumen of the stomach. The catheter and gastroscope are removed from the patient. This concludes the procedure.
Laparoscopic longitudinal gastrectomy (sleeve)
Laparoscopic longitudinal gastrectomy is a bariatric operation, the essence of which is to remove part of the stomach. Thanks to the operation, the size of the stomach is reduced tenfold. In addition, the part of the stomach removed during surgery is responsible for the production of the hormone ghrelin (the hunger hormone); a decrease in its concentration after surgery leads to a sustained decrease in appetite.
The essence of the operation
Longitudinal gastrectomy, or gastrectomy, is the most commonly performed operation in the world today. It has proven its safety and high effectiveness in the treatment of obesity. The duration of the operation is 1.5 - 2 hours. During this time, the surgeon removes part of the stomach (fundus and body) through small punctures, transforming its shape into a narrow tube while preserving all physiological valves. The result of the operation will be a reduction in the volume of the stomach, on average to 100–150 ml. Also in the removed part of the stomach there are zones for the production of the “hunger hormone” - ghrelin, which is responsible for regulating the feeling of hunger, this is an additional factor contributing to weight loss: in addition to reducing the amount of food consumed by almost 50%, changing the concentration of ghrelin reduces appetite and the need for constant intake food.
Longitudinal resection is an irreversible bariatric operation, unlike banding; here, changes are possible only in terms of subsequent translation of the results of the operation into gastric or biliopancreatic bypass.
Result
The average success rate of laparoscopic longitudinal gastrectomy is a loss of 60–75% of excess weight. Today, this type of surgical intervention is recognized as effective in world bariatric practice.
Peculiarities
1. Longitudinal resection is a fairly extensive surgical procedure. Therefore, the recovery period takes longer than with gastric banding. Typically the patient is in the hospital for 4–5 days. 2. The operation does not require further adjustment or the presence of a foreign body in the body, the results of the operation remain with the patient for life. 3. Full recovery after surgery takes about 2 months, this time is spent adjusting and then getting used to the new diet. Stomach surgery requires adherence to strict rules of food intake during this period in order to avoid postoperative complications and stress on the gastric sutures. 4. The patient, after longitudinal gastrectomy, must responsibly ensure that he receives adequate nutrition and a sufficient amount of microelements and vitamins. 5. One of the relative contraindications to longitudinal resection is disruption of the gastrointestinal tract (esophagus, stomach, duodenum). In some cases, it may be better to consider gastric bypass surgery.
How to live after installing a balloon
A few hours after installation of the balloon, the patient can go home, although many authors recommend staying in the clinic until the morning. The fact is that the first night after installing the balloon can be very unpleasant. There may be severe nausea and repeated vomiting. We must survive this first night. And if the patient remains in the clinic, he can be given a drip and given an injection of drugs for nausea and vomiting. If a person goes home, he will have to deal with it himself.
So, for the first 3 days the patient receives the following treatment.
- If there is repeated vomiting, 1.5 liters of Ringer's solution or saline is prescribed intravenously.
- In the presence of vomiting, Cerucal (metoclopramide) 2 ml (10 mg) 2 times a day intramuscularly. If there is no vomiting, Cerucal (metoclopramide) is prescribed in tablets of 10 mg three times a day.
- A very good medicine against nausea and vomiting is Torekan (thiethylperazine). It is prescribed in capsules of 6.5 mg three times a day. If there is severe vomiting, the drug can be administered into the rectum in the form of suppositories.
Every day, for the entire time the balloon is in the stomach (that is, 6 months), the patient should receive omeprazole 30 mg per day (1 tablet at night).
Unpleasant sensations in the stomach may remain for another 3-4 days, then the body adapts to the foreign body in the stomach, and the person stops feeling anything.
Nutrition with the balloon installed can, in principle, be normal, but it should be borne in mind that the best results were obtained if the patient consumed 1000-1500 kcal per day.
Adjustable gastric band
SUMMARY:
- After breastfeeding, it is necessary to adhere to a diet and physical activity
- Regular adjustment of the bandage's fullness will be required.
- When passing through a metal detector, the device’s reaction to the bandage may be detected
- It is necessary to introduce regular exercise into your schedule to maintain long-term results.
- Personal relationships may undergo significant changes after surgery
Bariatric surgery is just a tool to change your life . Long-term success requires diligence and a willingness to make changes in all areas of life.
Read the following sections for detailed information regarding diet and lifestyle after surgery.
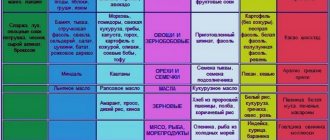
1. Power mode
| Time range | Diet requirements |
| 2-4 weeks before surgery | Gradual transition to proper nutrition |
| 2 weeks before surgery | Eating high in protein and low in carbohydrates, eliminating sugar from the diet |
| 1 week before surgery | Canceling permanent oral anticoagulant therapy and switching to injectable forms (more details about this can be found during the consultation) |
| 2 days before surgery | Clear liquids only |
| 12 hours before surgery | Do not eat or drink anything |
| 1 day after surgery | Clear liquids only |
| 2-7 days after surgery | Fruit juices, tea, protein shakes, low-fat milk + broths |
| 8-14 days after surgery 15-27 days after surgery | Adding pureed foods Soft foods that do not contain fiber |
| 4-5 weeks after surgery | Gradual transition to solid foods |
Remember: the diet in the early postoperative period is individual for each individual patient. Please discuss with your surgeon all the nuances of your diet and lifestyle after surgery.
2. Vitamin and mineral supplements
After surgery, LRB will need to take vitamin and mineral supplements in courses or (as recommended by a doctor) throughout life. This will help you avoid possible vitamin and mineral deficiencies associated with a decrease in the amount of food entering the body.
Here is a list of essential vitamins and minerals:
| Vitamins | Effect on the body |
| Multivitamins | Condition of the whole body |
| Calcium | Skeleton |
| Folate (folic acid) | The cardiovascular system |
| Iron | The cardiovascular system |
| Vitamin D | Condition of the whole body |
- Bandage correction
- The more full the band is, the sooner you feel full after eating. Excessive filling of the band can lead to reflux and vomiting, as well as vitamin and mineral deficiencies.
- It will take at least two adjustments to the bandage to determine the optimal fill level for you. When stabilizing body weight, fewer adjustments are required than during the period of active weight loss.
- By the 3rd year after surgery, as a rule, no more than 2-3 adjustments per year are required.
- Possible problems
- Metal detectors The risk of a signal occurring when passing through a metal detector is low. It depends on the sensitivity of the metal detectors and the presence of other metal objects passing through the metal detector, since it takes into account the total number of metal objects you have.
- Hand-held metal detector - possible alarm To avoid questions from security personnel, have a hospital discharge certificate with you to confirm the presence of a bandage that causes an alarm during the search.
- MRI machines – no contraindications
Despite the absence of contraindications to performing MRI after the installation of a bandage, inform the radiology specialist about the operation performed on you.
- Physical activity: 2.5-3 hours per week, distributed over 2-4 days
Training after LRB is essential to achieve long-term results in terms of weight loss.
Physical exercise ensures long-term results.
It has been proven that:
- Regular exercise provides greater weight loss and longer-term results
- There is an improvement in psychological well-being
- How often should you exercise?
Studies have shown that 2.5 hours of physical activity per week after LRB leads to 5.7% greater loss of excess body weight. It is advisable to exercise at the same time during the week - this will ensure regularity of training.
It is advisable to distribute 2.5 hours over 3 - 4 days a week (30 -45 minutes per day) - this will make training less tiring and at the same time allow you to develop endurance.
- Types of exercises
It is necessary to introduce 3 types of exercises into your workout:
- Endurance exercises - walking, cycling and especially swimming
- Stretching exercises. We recommend trying yoga classes as they include proper breathing techniques and bodyweight exercises for strength.
- Strength exercises - exercises on machines, with free weights and yoga
Click here to learn more about physical activity after surgery
- A new way of thinking and getting rid of food addiction
Food addiction
Our body is capable of producing certain hormones that cause hunger. Junk foods can alter hormonal signals, overstimulating your hunger center. The reaction to unhealthy food is similar to the body's reaction to taking drugs.
If food cravings are more important to you than:
- Personal health
- Family
- Friends
- Job
- Your appearance
- Health problems caused by obesity (diabetes, hypertension, obstructive sleep apnea)
…then most likely you are suffering from a food addiction.
Food addiction can lead to the development of obesity. If food addiction is not addressed after surgery, it can also lead to weight regain. If you think that you have a food addiction, seek advice from a psychologist - only working together with a specialist will help you cope with the problem of food addiction.
7. Relationships After Weight Loss The issue of changes in relationships after weight loss surgery is often overlooked by both patients and doctors. It is important to note that these changes can be both positive and negative, depending on the situation.
On the one hand, you will look and feel better after surgery. People you don't even know will treat you with more respect. They will look up to you. You will become physically attractive, sexy.
On the other hand , post-surgery patients are acutely aware of discrimination against people who are overweight, which can make them question whether this person could have treated me the same way if I hadn't lost weight. How can I fight obesity discrimination now that I'm on the other side of the fence?
In addition, people you have known for a long time may also change their attitude towards you. Could this make it awkward to interact with friends and family? Could your spouse or partner become more jealous?
If you have already dealt with the problem of relationships after surgery, help those who are yet to do so, tell your story here, share your experience with those who really need it.
You can discuss these and many other questions with our specialists
How does a person lose weight after installing a balloon?
Body weight loss begins immediately after installation of the balloon. On average, patients’ weight loss over 6 months looks like this (average data, analysis of results from several clinics):
- Patients lost from 0 to 40 kg
- Average weight loss was 15 kg
- Excess body weight decreased by 40%
- Body mass index decreased by 5.
Decrease in body mass index (BMI) against the background of standing balloon
Patients' adherence to diet influenced the results achieved:
- Patients who followed the diet and consumed 1000-1500 kcal/day lost an average of 18 kg.
- Patients who did not follow the diet lost an average of 9.6 kg.
This means that the patient's personality plays a big role in achieving the result. A person with high discipline who is willing to put in real effort to lose weight is likely to get better results than the patient who relies on the balloon to do everything for him. There are no miracles. All principles of weight loss, namely following a diet with limited fats and carbohydrates and reducing the total calorie content of food, and rational physical activity remain basic principles in the case of using a balloon. That is, a person loses weight through his own efforts, and the balloon only helps him.
SADI
SADI (Single Anastomosis Duodeno-Ileal bypass, or SADI-S, (Single Anastomosis Duodeno-Ileal bypass + Sleeve) is a new bariatric operation that is gaining increasing interest among our colleagues around the world. The SADI operation can be considered an advanced gastric bypass, Because it is intermediate between gastric bypass and gastric bypass surgery, the SADI operation takes the best from these operations and reduces the disadvantages of both bypass techniques.
As you know, BPS is the most powerful bariatric surgery, however, along with its high efficiency, it has a number of disadvantages. For example, a pronounced deficiency of protein, vitamins and micronutrients, which often cannot be corrected even by regular use of special medications, as well as extremely unpleasant intestinal phenomena in the form of constant diarrhea and socially unacceptable gas formation. This is because BPS is primarily a malabsorptive (working by limiting absorption in the small intestine) operation.
On the other hand, gastric bypass, which is primarily a restrictive surgery, generally does not have such problems, but sometimes its effect on weight, diabetes and dyslipidemia (high blood cholesterol and triglycerides) is insufficient. In addition, sometimes, in the long term, the effect of gastric bypass may be unstable.
The new SADI operation, proposed by our Spanish colleagues, is both restrictive and malabsorptive, and very interesting and favorable results have already been obtained with its use.
The SADI operation provides the same strong and stable effect on weight loss, diabetes and lipid disorders as BPS, and at the same time, such problems of BPS as uncontrolled metabolic disorders and intestinal problems (persistent diarrhea and socially unacceptable gas formation) for it. uncharacteristic.
The SADI operation consists of two components: a sleeve gastroplasty (SLIG) and a small bowel component, where only one anastomosis is performed between the duodenum and the small intestine (see figure). Thus, this operation can be used as an independent effective method of treating morbid obesity, and as an enhancing malabsorptive component in case of insufficient effectiveness of another popular bariatric intervention, sleeve gastrectomy.
Advantages of SADI surgery compared to gastric bypass:
- There is no disconnected part of the stomach that is difficult to control during SADI surgery (this is known to bother many patients after gastric bypass surgery)
- The pylorus (pylorus) is preserved, which is why there is no problem typical for gastric bypass surgery, such as dumping.
- There are almost never peptic ulcers of the anastomosis, which are possible with gastric bypass surgery
- Stronger and more stable effect compared to gastric bypass. Thus, according to Andrés Sánchez-Pernaute, almost all patients had 100% loss of excess weight at the 3rd year of observation (while with GS, on average, 80% loss of excess weight is achieved).
Indications for SADI surgery
- Patients with a BMI of 40 and above. It should be borne in mind that with a very high BMI and in poor health, SADI can be done in two stages (first DRAIN, then after weight loss, the intestinal stage to enhance and stabilize the effect). This approach really reduces the risk.
- Patients with type 2 diabetes mellitus (with a BMI of 30 or higher)
- Patients who have previously undergone sleeve gastroplasty - DRAIN surgery and who were unable to achieve the desired weight. In this case, DRAIN is complemented by the intestinal stage.
Removing the balloon
After 6 months, the balloon must be removed. If the patient does not tolerate the balloon well, removal has to be done earlier than planned.
How is the balloon removed? You need to come for removal on an empty stomach. The procedure is again done under complete anesthesia.
After sleep occurs, the doctor inserts a gastroscope into the stomach for examination. Interestingly, while it is in the stomach, the balloon changes its color - instead of white and transparent, it becomes brownish. This is due to the fact that the wall of the balloon is stained with bile pigments. The balloon is pierced with a needle and the liquid is sucked out of it. After the fluid is sucked out, the balloon collapses. After this, the empty balloon is removed together with a gastroscope using a special clamp. The picture below shows the balloon after it has been removed from the stomach.
2-3 hours after removal of the balloon, the patient can go home; there is no need to stay in the clinic overnight.
On this day, however, you should not drive a car yourself.
Biliopacreotic shunting
Biliopancreatic bypass conventionally includes 2 types of bariatric operations: longitudinal gastrectomy (or drainage) and reconstruction of the intestinal anatomy. Thanks to this, a sustainable reduction in excess weight is achieved up to 70–80% or more, regardless of the caloric content of the diet.
The essence of the operation
Biliopancreatic bypass uses 2 mechanisms of weight loss at the same time: removing part of the stomach triggers a restrictive mechanism (reducing the volume of the stomach leads to a decrease in the amount of food ingested), and separating the routes of food and digestive juices by forming separate intestinal loops activates the malabsorptive mechanism (changes in food digestion and absorption nutrients).
During the operation, the surgeon removes the gallbladder - this is necessary to prevent stone formation, which inevitably occurs due to changes in digestive processes. If the BMI is significantly higher than the body mass index (super-obesity) or there are relative contraindications, the operation can be performed in 2 stages. This intervention has been performed since the mid-70s in patients with severe forms of obesity and in obese patients with concomitant pathologies.
Result
Biliopacetic bypass surgery provides a fairly quick and stable result in reducing excess weight up to 80 - 95% with the ability to achieve ideal weight, shows 99% effectiveness in the treatment of type 2 diabetes, as well as a pronounced reduction in the risk of cardiovascular diseases due to a significant decrease in the concentration of cholesterol in blood.
Peculiarities
1. Biliopacreatic bypass surgery is the most complex bariatric operation and at the same time the most effective for patients with morbid obesity complicated by type 2 diabetes mellitus. 2. The operation lasts 3.5 - 4 hours, the patient is discharged from the hospital 5-6 days after the operation. 3. Volumetric restructuring of the digestive tract requires long-term recovery (2–3 months), compliance with postoperative dietary restrictions to avoid complications. 4. Patients after biliocreatic bypass surgery must take multivitamin complexes, microelements and nutritional supplements for life.