Causes of gynecomastia in men
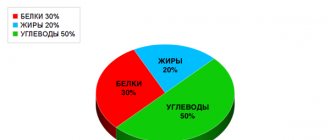
The development of breast tissue depends on the influence of sex steroids. Normally, a man's body produces estrogens and testosterone, but their ratio differs from that of women in favor of androgens. The main mechanisms of changes in hormone concentrations are associated with the following factors:
- excessive synthesis of estrogen, more often observed in tumor tissues;
- violation of hormone inactivation, occurs in liver pathology;
- changes in steroid metabolism.
If in adolescents gynecomastia can be associated with physiological changes in the body and maturation, then in men the cause of the condition is most often pathological deviations in the balance of estrogen. Their concentration exceeds the norm, sometimes several times, in the following cases:
- estrogen-producing Leydig cell tumors in the testes;
- taking steroid hormones to increase muscle mass and create body contour;
- treatment with certain groups of drugs;
- use of opiate drugs.
Treatment with cytostatics, antidepressants, antifungals and some antiviral drugs used for HIV infection can lead to gynecomastia in men. “Excess estrogen leads to the development of mammary gland tissue in men and the development of gynecomastia. As a rule, this happens in the case of teenage hormonal disorders, obesity and taking anabolic steroids!” A relative imbalance of hormones can cause the development of gynecomastia in an adult man. In this case, the concentration of estrogen remains normal, but their relationship with progesterone is disrupted. This is possible in the following conditions:
- age-related changes in the structure of the testicles, physiological decline in testicular function;
- liver diseases that impair its function, including cirrhosis;
- patients with renal failure who regularly undergo hemodialysis;
- hypogonadotropic hypogonadism – testosterone synthesis is inhibited, but estrogen is retained;
- endocrine diseases - hyperthyroidism, hyperprolactinemia.
Obesity, especially in older men, often also leads to the development of gynecomastia.
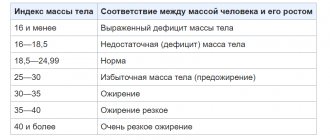
Types of obesity
There are 3 types of obesity: abdominal (fat deposition in the abdomen and upper torso), gynoid (fat deposition in the buttocks and thighs) and mixed.
To understand what type of obesity you have, you need to determine your waist and hip circumferences and calculate their ratio. Waist circumference (WC) is measured below the lower edge of the ribs above the navel. The circumference of the hips is in their widest area at the level of the buttocks. The OT indicator of 94 cm in men and 80 cm in women is characteristic of the abdominal type of obesity (apple type) and is synonymous with a high risk for your health.
A WC/TB ratio exceeding 1.0 in men and 0.85 in women indicates an abdominal type of obesity.
Excess body weight is not only a cosmetic defect. Obesity creates many problems: with every extra kilogram, a piece of health is lost.
It should be remembered that obesity in general and the abdominal distribution of adipose tissue in particular are independent risk factors for the development of many diseases. Moreover, the abdominal type of distribution of adipose tissue, even with a slight increase in body weight, already poses a threat to health. Visceral adipose tissue has a different sensitivity to hormonal influences that regulate changes in lipid storage and metabolism. Visceral fat deposition correlates with metabolic abnormalities in the body - insulin resistance, hyperinsulinemia, IGT, hypertriglyceridemia, increased LDL cholesterol fractions and a decrease in HDL cholesterol, while total blood cholesterol may remain relatively low.
Possible complications of obesity affect almost all human internal organs and body systems - cardiovascular, respiratory, reproductive, etc., metabolic processes are disrupted.
- Cardiovascular : arterial hypertension - high blood pressure for a long time;
- heart failure - the inability of the heart to fully perform its function;
- stroke - brain damage as a result of acute cerebrovascular accident;
- myocardial infarction - death of a section of the heart muscle; Varicose veins.
- non-insulin-dependent diabetes mellitus - a disorder of carbohydrate metabolism;
- shortness of breath - rapid breathing;
- arthritis - inflammation and pain in the joints;
- gallstone disease - the formation of stones in the gall bladder.
- menstrual irregularities;
- increased risk of developing cancer: breast; ovaries, cervix; prostate gland; rectum.
Clinical studies have confirmed that body weight is an important prognostic criterion for increased mortality in young and middle age, both among men and among women.
The most serious diseases that develop in connection with obesity are arterial hypertension, diabetes mellitus and atherosclerosis. They can significantly reduce your quality of life, leading to disability and premature death.
In obese people, high blood pressure is 5 times more common than in people of normal body weight. And the assertion that weight loss in obese people is the most effective form of treatment for hypertension is completely justified. Your body can only cope with a temporary increase in blood pressure levels. Constant high blood pressure leads to dysfunction of the heart, kidneys, and brain. Losing weight, even 5 kilograms, improves blood pressure!
Obesity is often accompanied by the development of metabolic syndrome and diabetes. Metabolic syndrome is a complex of interrelated disorders of carbohydrate and fat metabolism, as well as mechanisms of regulation of blood pressure (BP) and endothelial function, the development of which is based on a decrease in tissue sensitivity to insulin - insulin resistance. Of course, not every obese person gets diabetes. For its occurrence, hereditary predisposition, age, sedentary lifestyle, and diet are of great importance. But obesity, its duration and severity are of decisive importance in the development of diabetes mellitus. Insulin resistance is directly related to abdominal obesity and is the cause of hyperinsulinemia and type 2 diabetes mellitus. Among patients suffering from non-insulin-dependent diabetes mellitus, 80% are overweight or obese. If you are obese or overweight, you need to regularly check your blood glucose levels.
You are obese. Increasingly, you are bothered by a headache, a feeling of heaviness in the chest, your legs swell in the evening, and shortness of breath appears when climbing stairs. These symptoms indicate disturbances in the functioning of the cardiovascular system. Or it could be like this: against the background of good health, a myocardial infarction or stroke suddenly develops. The main cause of all adversity is atherosclerosis. Atherosclerosis is a systemic disease that affects the arteries, or blood vessels. The walls of blood vessels become denser due to the deposition of cholesterol in them if it is found in excess in the blood. Atherosclerotic plaques form, which gradually increase and multiply, thereby narrowing the lumen of the arteries, impeding blood flow. As blood flow slows down, there is a risk of blood clots forming. Blood clots further disrupt normal blood circulation. Thus, less and less oxygen and nutrients reach the organs and tissues, and all the cells of your body. At this stage, atherosclerosis, which until now has been secretive and asymptomatic, makes itself known. The main culprit in the development of atherosclerosis is cholesterol. The same cholesterol that is an essential component of the outer membranes of all cells in our body. The same cholesterol, without which the formation of hormones is impossible. But everything is good in moderation, and even more so cholesterol, which we consume directly from food of animal origin and especially from fats. When the measure is violated, the development of atherosclerosis accelerates.
Excess body weight and obesity are significant risk factors for the development of gastroesophageal reflux disease, erosive esophagitis, manifested by despotic disorders (belching of eaten food and air, bitterness in the mouth, nausea, night cough, hoarseness, reflux-associated bronchial asthma). The target organ for obesity is the liver, non-alcoholic fatty liver disease (NAFLD) is formed, NAFLD is associated with obesity, and inflammation: insulin resistance leading to oxidative stress, endothelial dysfunction, chronic inflammation; obesity leads to an increase in the size of the liver, mainly its left lobe, disruption of biochemical liver parameters, changes in the structure of the organ (steatosis, fibrosis, cirrhosis).
Currently, the problem of pelvic floor dysfunction has acquired particular relevance and social significance: every third woman suffers from prolapse and prolapse of the pelvic organs, urinary and fecal incontinence, and, consequently, problems in sexual life. Predictors of the development of pelvic dysfunction include pregnancy, childbirth with a long period of expulsion and a large fetus), birth trauma, damage to the pelvic nerves and muscles, and surgical interventions on the pelvic floor. However, the main provoking factors are chronic constipation, some somatic diseases and mainly obesity. An increase in body mass index by 5 units increases the risk of developing urinary incontinence by 60-100%, and a decrease in body weight by 5-8% leads to a reduction in the frequency of episodes of urinary incontinence of various origins by 50-70%.
Compared with the general population, individuals with extreme obesity have an increased incidence of anxiety, depression, and sleep disturbances. 50% of people with a body mass index over 40 have at least one mental disorder. The prevalence of depression in the population is 17%, and the prevalence of obesity in streets is 29-56%.
The risk of carcinogenesis in postmenopausal women is 20% greater in individuals with obesity than in those without it; in addition, obesity is associated with a large tumor size; the presence of obesity worsens the prognosis of the disease.
According to modern opinion, adipose tissue is an independent active endocrine organ that secretes a number of hormones and enzymes, inflammatory cytokines. One of the important features of adipose tissue is the presence in it of the aromatase enzyme, which converts testosterone into estradiol, as well as the presence of receptors for sex steroid hormones (estrogen, testosterone, progesterone). Obesity is accompanied by suppression of ovarian steroidogenesis and decreased production of estradiol by granulosa cells. In this case, the development of follicles stops, the level of sex steroid binding globulin decreases, the secretion of gonadotropins is disrupted, and the level of sex hormones decreases. In women, the main manifestations are: irregular menstrual cycle, hypomenstrual syndrome, secondary amenorrhea, acyclic bleeding against the background of hyperplastic processes in the endometrium, high incidence of infertility. According to research data, every 3rd woman who seeks medical help with the problem of MC disorders and infertility is overweight, and every 5th is obese. Abdominal adipose tissue, neurohormonal disorders accompanying abdominal obesity, and increased activity of the sympathetic nervous system play an important role in the development and progression of insulin resistance and associated metabolic disorders, with subsequent excessive secretion of insulin into the blood, which leads to hyperinsulinemia. Insulin resistance lies in the development of many diseases of the reproductive system, such as polycystic ovary syndrome (PCOS) and infertility. Obesity and insulin resistance are closely associated with the development of systemic oxidative stress, which has a multifaceted negative impact on the reproductive system, including the development of mitochondrial dysfunction of the egg and follicular oxidative stress, regardless of whether a woman has PCOS, which increases the risk of miscarriage. There is a direct relationship between an increase in body weight and the severity of ovarian disorders, accompanied by anovulation, inferiority of the luteal phase and a decreasing frequency of pregnancies. With a BMI of more than 29 kg/cm², each kilogram gained reduces the possibility of spontaneous pregnancy by 4%.
Vitamin D
Adipose tissue plays an important role in the regulation of phosphorus-calcium metabolism (the initial stages of vitamin D formation) and the metabolism of sex steroids (aromatase in fat cells promotes the conversion of adrenal androgens into estrogens).
When assessing vitamin D deficiency in various ethnic and age groups, a relationship was identified between obesity and vitamin D deficiency. Obesity is one of the factors for vitamin D deficiency and in the development of secondary hyperparathyroidism (SHPT), a more pronounced deficiency is experienced by people suffering from morbid obesity. SHPT in obese individuals in the absence of CKD or other somatic diseases may be considered a consequence of long-term vitamin D deficiency and hypocalcemia.
Vitamin D is present in a very limited amount of food, and its synthesis in the body is possible only when the skin is exposed to ultraviolet sunlight. Vitamin D promotes the absorption of calcium in the intestine and maintains adequate levels of calcium and phosphate in the blood to promote bone mineralization and prevent hypocalcemic seizures. It plays a major role in the prevention of rickets in children and osteomalacia in adults, and is necessary for bone growth and the process of bone remodeling. The function of vitamin D also affects neuromuscular conduction, immunity, and inflammation. Vitamin D is an important part of homeostasis: it reduces the risk of developing autoimmune pathologies and reduces the risk of infections. An important aspect is the interaction of the vitamin with the renin-angiotensin system - leveling molecular and clinical markers in diabetic nephropathy, reducing proteinuria, high blood pressure, inflammation and fibrosis. Vitamin D deficiency causes the development of myopathy, which is manifested by muscle weakness, difficulty walking, and many cases of falls and fractures in older people; It is also a predictor of cardiovascular accidents, dyslipidemia, and arterial hypertension. It plays an important role in reproductive health: with a deficiency, polycystic ovary syndrome is observed, the qualitative and quantitative characteristics of sperm and testosterone levels decrease. During pregnancy, vitamin D deficiency is associated with adverse outcomes: risk of preeclampia, infections, premature birth, cesarean section, gestational diabetes, and development of rickets in the child.
Signs of gynecomastia in men
In adulthood, a man notices that one or both mammary glands begin to increase in size. More often the process begins in the area around the nipple of the areola. They protrude above the surface of the chest.
Men with gynecomastia may complain of breast tenderness and engorgement, but this is not necessarily a sign. The skin in the area of pathological enlargement remains healthy, there is no discharge from the nipple. Most men find it difficult to answer how long this condition lasts.
Gynecomastia in most cases accompanies other diseases or is their consequence. Therefore, additional symptoms may be of concern:
- decreased libido;
- deterioration of erection;
- female type of fat deposition;
- infertility.
“When diagnosing gynecomastia, the doctor must determine the leading factors that caused the disease.”
Gynecomastia does not threaten a man’s life; more often it is a cosmetic defect. But with unilateral breast enlargement, with the appearance of discharge, changes in the skin over the tumor, the likelihood of a malignant process is high.
Gynecomastia in men on ultrasound
Gynecomastia can be suspected upon examination and palpation of the mammary gland. But to confirm the diagnosis, an ultrasound examination is necessary. Ultrasounds are performed for men with gynecomastia at any convenient time, unlike women with breast pathology.
Special preparation for ultrasound for gynecomastia is not required. The patient is examined alternately in a supine position with arms thrown back and sitting. The ultrasound probe is carried out in a fan-shaped manner in the direction from the areola to the periphery of the mammary gland. All sectors of the chest are sequentially examined, imagining it as a conventional dial.
After examining the breast parenchyma, they proceed to assessing the areola. It is quite dense, so it does not transmit ultrasonic waves well. To study the tissue behind it, the sensor is installed on the side and the rays are directed into the subareolar space.
An ultrasound of the mammary gland is concluded by examining regional lymph nodes located in the supra- and subclavian, axillary regions and in the parasternal lines. This eliminates the possibility of metastases from malignant tumors.
Ultrasound evaluates the structure of a neoplasm in the mammary gland according to standard criteria. Gynecomastia is a nodular formation that is clearly visualized using ultrasound. During the examination, the doctor can determine the shape, size, spatial orientation and location of the node. The following features are characteristic of gynecomastia in men:
- the node is located in the retroareolar region or in the subcutaneous fat of the breast;
- the shape of the node is often polygonal, but there are ovoid, flat, ellipsoidal variants;
- the contours of the node may be unclear, echogenicity is reduced;
- the structure of the node is heterogeneous due to isoechoic and hyperechoic areas in the form of linear, point formations, but they do not have signs of pathological inclusions. Hyperechoic areas are areas of fibrous tissue;
- with gynecomastia, the ducts of the gland are rarely visualized; microcalcifications and cystic cavities are sometimes encountered.
Dopplerography for gynecomastia and color Doppler mapping are uninformative and not indicative. The vessels can be located either intranodular or perinodular. Gynecomastia is characterized by venous blood flow, but sometimes arterial blood flow occurs.
“When examining men with gynecomastia, mammography is not used. This method is not very informative due to the structural features of the neoplasm and its localization behind the nipple.”
Early signs
Unlike most diseases associated with a violation of the number of chromosomes, the intrauterine development of children with Klinefelter syndrome proceeds normally, and there is no tendency to premature termination of pregnancy. So in infancy and early childhood it is almost impossible to suspect pathology. Moreover, clinical signs of classic Klinefelter syndrome usually appear only in adolescence. However, there are symptoms that suggest the presence of Klinefelter syndrome in the prepubertal period:
- high growth (peak height increase occurs between 5–8 years);
- long legs (disproportionate physique);
- high waist.
Some patients experience some delay in speech development.
In adolescence, the syndrome often manifests itself as gynecomastia, which with this pathology has the appearance of bilateral symmetrical painless enlargement of the mammary glands. Since this type of gynecomastia is often observed in completely healthy adolescents, this symptom often goes unnoticed. Normally, teenage gynecomastia disappears without a trace within several years, but in patients with Klinefelter syndrome, reverse involution of the mammary glands does not occur. In some cases, gynecomastia may not develop at all, and then the pathology manifests itself as signs of androgen deficiency already in the postpubertal period.
Additional diagnostics for gynecomastia
Gynecomastia in men is accompanied by diseases of the endocrine system and internal organs. Therefore, during the examination it is necessary to find the reasons for the appearance of the node. When you first visit a doctor, the external genitalia are examined. If gynecomastia is associated with insufficient testosterone production, the doctor may detect testicular hypoplasia or, conversely, their enlargement due to the formation of a tumor.
Laboratory diagnosis includes determination of hormone concentrations. The attending physician individually determines which indicators the patient needs. It can be:
- testosterone;
- estradiol;
- progesterone;
- hCG;
- prolactin;
- luteinizing hormone;
- cortisol;
- thyroid hormones.
The cause of gynecomastia in a man must be sought in order to reduce the likelihood of relapse of the disease. Therefore, they may additionally prescribe a CT or MRI of the brain, ultrasound of the abdominal cavity and thyroid gland, and a biochemical blood test.
To determine the morphological characteristics of the node tissue, a biopsy is performed under ultrasound guidance.
Diagnosis of Klinefelter syndrome
In many countries, Klinefelter syndrome is often diagnosed before the birth of a child, since many women of late childbearing age, due to the high risk of genetic defects in future offspring, use prenatal genetic diagnosis of the fetus. Often, prenatal detection of Klinefelter syndrome is a reason for termination of pregnancy, including on the recommendation of doctors. In Russia, analysis of the karyotype of an unborn child is extremely rare.
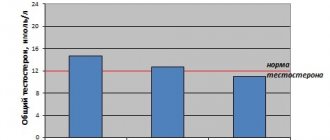
If Klinefelter syndrome is suspected, a laboratory blood test is performed to determine the level of male sex hormones. Differential diagnosis with other diseases that occur with manifestations of androgen deficiency is necessary. An accurate diagnosis of Klinefelter syndrome is made based on studying the karyotype (set of chromosomes) of the patient.
Tests needed to confirm the diagnosis
| Analyzes | results |
| Karyotype | 47,ХХY (80% of cases) 48,ХХYY 48,ХХХY 49,ХХХY 46,ХY/47,ХХY |
| Concentration of LH, FSH | Increased, especially FSH |
| Total testosterone concentration | Most often reduced (in some cases normal due to an increase in sex steroid-binding globulin SSSG or at the initial stage of disease development) |
In all men with sharply increased concentrations of gonadotropins, it is necessary to exclude Klinefelter syndrome, since often the first laboratory sign of this genetic pathology is an increase in the concentration of gonadotropins in the blood with normal levels of total testosterone.
Klinefelter syndrome must be differentiated from other forms of primary hypogonadism. In any case, if the level of FSH in the blood increases, it is necessary to determine the karyotype to exclude, first of all, Klinefelter syndrome.
Classification of gynecomastia in men
Already during an ultrasound of the breast, the type of gynecomastia can be determined. In clinical practice, several classifications of pathology are used. Depending on the tissue origin, the following types of pathology are distinguished:
- true - formed from the lobar milk ducts and hypertrophied fibrous tissue;
- false – it is based on hypertrophy of adipose tissue;
- mixed - the formation of a pathological node occurs due to adipose and fibrous tissue.
Based on histological examination, it is possible to determine the stage of development of gynecomastia and draw up a treatment plan for the patient. The following stages of node formation are distinguished:
- proliferation - at the initial stage, changes in the mammary gland are reversible, therefore conservative treatment is effective. The stage lasts up to 4 months;
- intermediate stage - connective tissue matures in the node, it compacts the structure. The duration of the intermediate period is up to 1 year;
- fibrosis - a node has formed, there is a lot of connective tissue in it, fatty tissue is deposited around the glandular tissue. Regression of the disease is impossible.
When classifying the degree of mammary gland enlargement in men, the size of the areola and its relationship with the node are taken into account. There are 4 degrees of gynecomastia:
- There is minimal nodularity under the areola.
- The diameter of the node is smaller than the areola.
- The size of the node is equal to the diameter of the areola.
- The tumor is larger than the areola.
Also, based on a histological examination, the doctor receives confirmation of the benign nature of the neoplasm. But in conclusion, the degree of proliferation of the epithelium can be described, by which one can judge the likelihood of developing a malignant neoplasm. If proliferation is not observed, then the risk of developing breast cancer in a man with gynecomastia is increased by 1.5 times compared to a healthy person. When foci of proliferation are detected, the probability of developing a malignant tumor increases up to 1.9 times. In the case of atypical proliferation, the risk of breast cancer increases by 3-25 times.
History of the discovery of the syndrome
The syndrome got its name in honor of Harry Klinefelter, a doctor who first described the clinical picture of the disease in 1942. Klinefelter and colleagues published a study of 9 men with common symptoms such as low body hair, eunuchoid body type, tall stature, and small testicles. Later, in 1956, geneticists Plunkett and Barr (E.R. Plunkett, M.L. Barr) discovered sex chromatin bodies in the nuclei of cells of the oral mucosa in men with Klinefelter syndrome, and in 1959 Polanyi and Ford (P.E. Polanyi, SE Ford) and colleagues showed that patients have an extra X chromosome in their chromosome set.
Active research into this pathology was conducted in the 70s in the USA. Then all newborn boys were subjected to karyotyping, as a result of which it was possible to reliably identify the prevalence and genetic characteristics of Klinefelter syndrome.
Interestingly, mice can also have XXY sex chromosome trisomy, making them useful models for studying Klinefelter syndrome.
Treatment of gynecomastia in men
The doctor chooses a treatment method depending on the causes of the pathology and the stage of gynecomastia. If the node is still at the proliferation stage, it can be eliminated conservatively. To do this, it is necessary to find the cause of absolute or relative hyperestrogenism.
An endocrinologist can be involved in the treatment of gynecomastia. In patients with thyroid diseases, it is necessary to monitor and adjust hormone levels. In case of alimentary obesity, the diet is adjusted, and sometimes medications are prescribed to control appetite or the absorption of carbohydrates and lipids.
“If gynecomastia has developed due to the use of medications, the use of anabolic steroids, for successful treatment it is necessary to discontinue or replace the drugs with safer ones.”
But given that most men do not seek medical help when the first signs of gynecomastia appear, conservative treatment becomes impossible. Therefore, the main method of treating gynecomastia in men is surgery.
Surgery for gynecomastia in men
Gynecomastia is a benign formation that rarely leads to the development of complications in men. Therefore, the main indication for surgery is a cosmetic defect that causes psychological discomfort to the patient.
Preparation for surgery is carried out according to the standard procedure. An examination for HIV, syphilis, hepatitis, an ECG, a clinical examination of blood and urine is required. Diagnostics are carried out to determine contraindications for surgery and the patient’s condition.
The operation is performed by subcutaneous mastectomy if true gynecomastia is diagnosed. For patients with false gynecomastia, the doctor may suggest performing liposuction and removing fat tissue in a minimally invasive way. But this method is accompanied by frequent relapses, especially in patients who have not eliminated the cause of the pathology.
For mixed types of gynecomastia, a combination of liposuction and mastectomy can be used. This increases the likelihood of a favorable outcome and reduces the chances of relapse. In advanced forms of gynecomastia, when a large nodule has formed and the skin on the mammary gland has stretched, the operation is carried out in 2 stages - first the nodule is removed, then breast plastic surgery is performed.
To remove fatty tissue, 2 punctures on each side of the mammary gland are enough. But the node with gynecomastia is quite dense, it cannot be aspirated. Therefore, for a mastectomy, an incision is made under the areola, equal to ¼ of its circumference. Through it, the node is carefully isolated and separated from the surrounding tissues.
“To exclude a malignant tumor, it is necessary to send the removed material for histological examination.”
Recovery after surgery
In the first few days after the operation, you will be bothered by pain in the mammary gland and its swelling. But they go away if you use compression garments for 2 weeks. To reduce pain, non-steroidal anti-inflammatory drugs are prescribed.
Complications after surgery are rare. In the first 3 weeks there is a risk of breast seroma formation. Therefore, periodic observations by a mammologist are recommended. Bruising after surgery for gynecomastia goes away on its own and does not require special treatment.
A rare complication is impaired blood flow or lymphatic drainage in the breast and areola area. If the doctor follows the surgical technique, these undesirable effects are excluded.
Rough scars form in patients prone to keloid formation. In older men, surgery does not always provide a good cosmetic effect. Therefore, subsequent plastic surgery may be required.
Prevention and prognosis
For men diagnosed with gynecomastia, the prognosis is favorable. The development of a malignant breast tumor occurs in only 1% of patients. After treatment, if the doctor’s recommendations are followed and the underlying disease is treated, the re-formation of gynecomastia in men does not occur.
To prevent hypertrophy of breast tissue, it is necessary to exclude factors in life that cause relative or absolute hyperestrogenism. To do this, men need to adhere to proper nutrition, not abuse alcohol, and not use drugs. For those involved in bodybuilding, the use of anabolic steroids should be approached with caution or not.
Stress affects the state of the hypothalamic-pituitary system, which regulates the activity of the gonads. Therefore, against the background of constant mental stress, hormonal problems may worsen.
At our Mammology Center, doctors have extensive experience in diagnosing and treating gynecomastia in men. We use modern ultrasound machines to diagnose pathology as accurately as possible. You can make an appointment by calling the numbers listed on the website or using the feedback form.